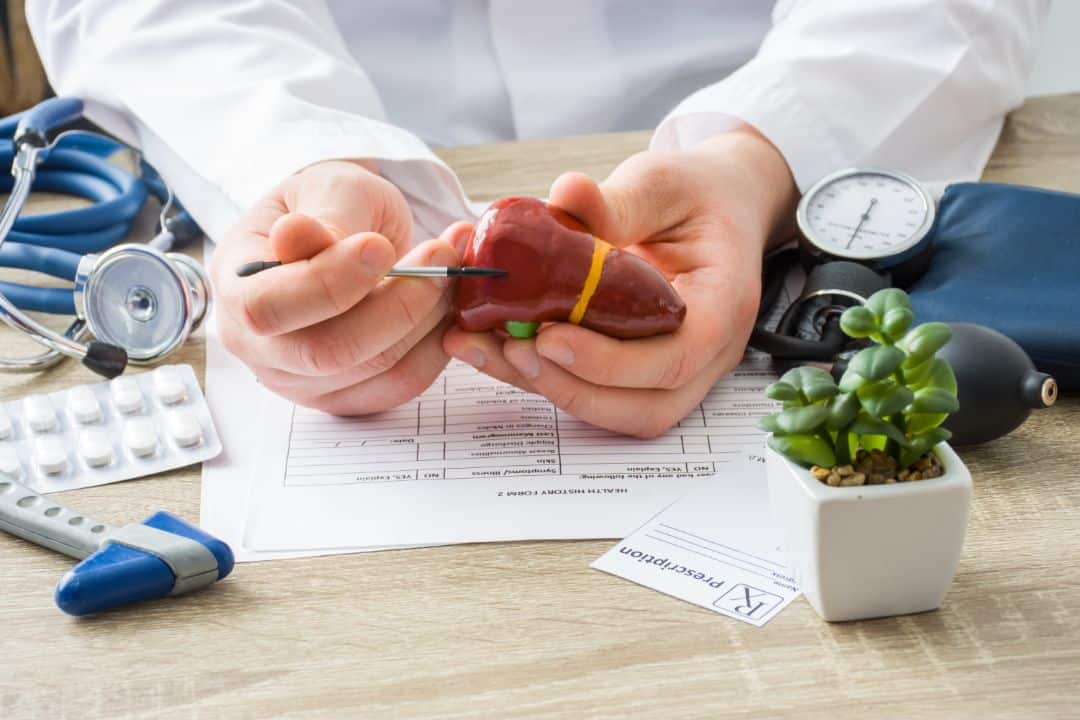
The liver is a parenchymal organ (filled with tissue, enclosed by a capsule), vital for human survival. The functions of this organ are numerous, with over 500 believed to exist in our body. Some of these functions include:
- Metabolic functions (it processes nutrients from food to create proteins necessary for the development and functioning of the body’s defense mechanisms).
- Production of bile, which helps eliminate unnecessary substances and aids in the breakdown of ingested fats.
- Detoxification, achieved through blood filtration and removal of toxins.
Due to its involvement in numerous processes in the body, the liver is exposed to hazardous agents and is susceptible to diseases. Viral infections, excessive alcohol consumption, smoking, use of narcotics, a diet high in fat, tumors, toxic damage, and the accumulation of iron or copper are just some of the risk factors that can lead to liver damage, hindering the organ from performing its vital functions.
What Kind of Liver Diseases Are There?
Liver diseases can manifest in various ways. Patients may complain of:
- Dull pain and discomfort below the right ribcage.
- Enlargement of the liver, sometimes palpable by the patient.
- Loss of appetite, nausea, and vomiting.
- Sudden weight loss.
- Dark urine and extremely pale (white) stools.
- Appearance of swelling in the abdomen or extremities.
- Yellow discoloration of the skin and whites of the eyes accompanied by itching.
Diagnosis
In the case of any of these complaints or a combination of them, it is necessary to consult a doctor. Following the doctor’s advice, blood tests, complete blood count, levels of bilirubin and liver enzymes, as well as levels of tumor markers, should be checked if there is suspicion of a malignant tumor.
In line with the results, some of the radiological examinations, such as ultrasound (with or without elastography for liver tissue), CT scans, and MRI scans of the abdomen, may be indicated.
Liver Disease Prevention:
- Eat a healthy and diverse diet while avoiding fatty foods;
- For those with a history of liver tumors, undergo regular check-ups as advised by the doctor;
- Maintain the recommended body weight;
- Consume moderate amounts of alcohol or avoid it entirely;
- Use medications strictly according to the doctor’s instructions;
- Practice safe sexual behavior;
- Avoid contact with someone else’s blood or body fluids.
When Is an Examination and Surgical Intervention Necessary?
Surgical treatment is indicated for liver tumors, symptomatic liver cysts causing issues in patients, and patients with liver failure requiring transplantation.
Liver tumors can be primary, originating from the liver tissue itself, or metastatic.
Primary Liver Tumors
The most common primary liver tumors are hepatocellular and cholangiocellular tumors, but there are also mixed forms with characteristics of both.
Hepatocellular carcinoma is significantly more common, diagnosed in about a million people worldwide every year. A risk factor for hepatocellular carcinoma is liver cirrhosis due to excessive alcohol consumption or viral infection (hepatitis). Only about 20% of these tumors occur in patients without liver cirrhosis.
It is characterized by aggressive biology with rapid disease progression, making early-stage diagnosis crucial, especially in patients who haven’t developed symptoms yet. This can only be achieved through strict screening programs for patients with liver cirrhosis and other risk factors. Due to the usually advanced stage at which patients present, only 10-30% of patients are diagnosed at a stage where surgical removal of the tumor is possible.
Factors influencing the decision on whether the patient can undergo surgery include:
- Patient’s condition (presence of other diseases, age)
- Liver condition (functional reserve of the cirrhotic liver)
- Stage of the disease (number and size of tumor nodules)
Primary liver tumors require anatomical liver resections (removal of the entire or multiple segments of the liver), emphasizing the importance of treatment by an experienced hepatobiliary surgeon.
Secondary (Metastatic) Liver Tumors
Secondary (metastatic) liver tumors occur due to the spread of tumors from other locations to the liver. Because of the liver’s specific vascularization (having both arterial and venous circulation), tumors from all abdominal and pelvic organs can affect this organ by spreading. About 80% of liver metastases originate from adenocarcinomas, most commonly colorectal, followed by gastric, pancreatic, and others…
If metastases develop in the liver, symptoms can vary depending on their number and location. Patients most commonly report pain and discomfort below the right ribcage, jaundice, abdominal swelling due to the accumulation of free fluid, weakness, loss of appetite, weight loss, etc.
Treatment of Liver Tumors
Metastatic liver disease can be treated in various ways, depending on the timing of metastasis detection, whether synchronous (at the same time as the primary tumor) or metachronous (after the surgery and treatment of the primary tumor).
Synchronous presentation is usually initially treated with chemotherapy and targeted biological therapy for better long-term disease control, followed by surgery. When surgically treating liver metastases, a sparing approach is used whenever possible, removing the metastasis with the surrounding liver tissue. This is not achievable if the tumor’s position jeopardizes any of the liver’s blood vessels, requiring more extensive (larger) liver resection.
Liver cysts require surgical treatment if it is a case of hepatic echinococcosis. Patients with simple liver cysts are also operated on when, due to their significant size, they exert pressure on surrounding organs, leading to issues that affect the patient’s quality of life.
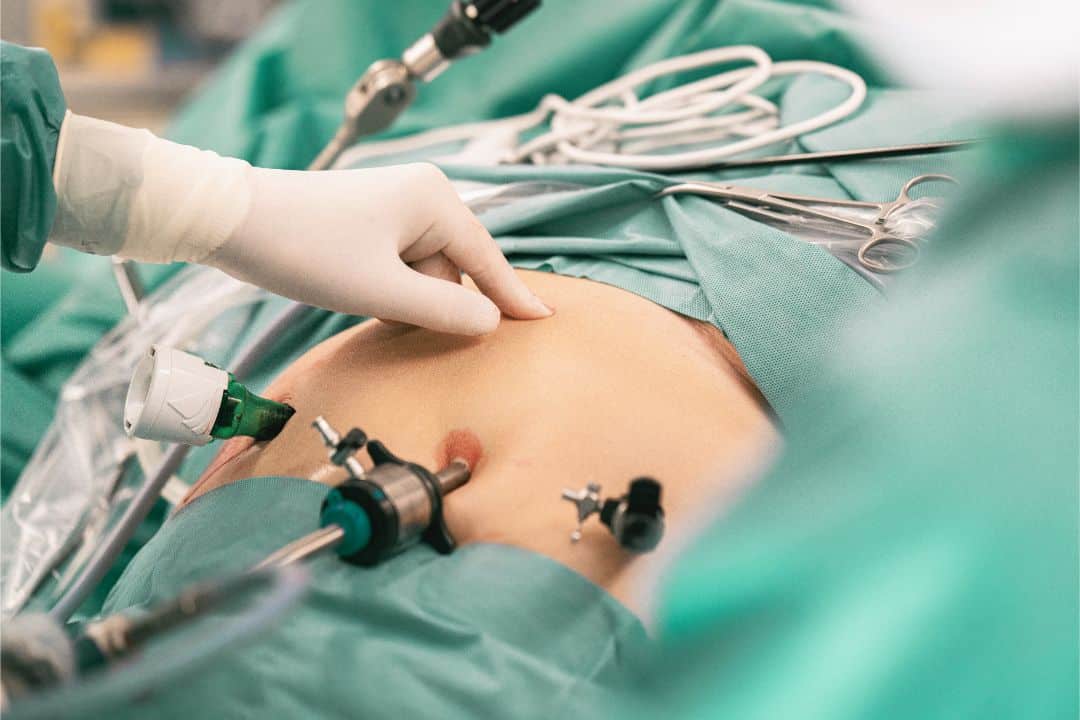
Minimally Invasive Laparoscopic Liver Surgery
All the mentioned surgeries can technically be performed using a minimally invasive approach (laparoscopic) if there are no clear contraindications.
Laparoscopy is a technique that provides access to the abdominal cavity through small incisions in the abdominal wall, ranging in size from 5 to 12 mm. Through specially made working channels (ports), and with the help of elegant instruments and a camera with magnification of 5 to 10 times, we can access every part of the abdominal cavity and chest, adequately identify and solve the problem. These small incisions, compared to traditional surgeries, offer the possibility of rapid recovery, reduce the risk of infection, allowing a return to regular activities within a few days. The advantage of the magnifying camera minimizes the possibility of errors in experienced hands, leading to the observation of the smallest details during the procedure.